When Diana Crouch found out she was pregnant, she started taking every precaution she could to keep herself and her baby safe. She exercised often, drank water and tried to eat right. She even stopped using her usual facial cleanser because she was worried about the chemicals.
So when her doctor talked to her about getting vaccinated for COVID, she balked.
“I just didn’t want to risk it,” she said. “I was like, we have an immune system for this, and I don’t want to do anything that might affect my baby. ”In April 2021, when Diana got pregnant, less than 20% of pregnant people nationwide were vaccinated for COVID. Now, more than 65% of pregnant people are vaccinated, but OB-GYNs say they’re still battling significant fear and misinformation.
Time and again, they say, patients tell them the chance of complications from the vaccine is too high, and the chance of getting seriously ill from COVID is low.
But that is a complete inversion of reality.
“We have so much data that [the vaccine] has been shown to be safe in all three trimesters of pregnancy,” said Manisha Gandhi, chief of maternal fetal medicine at Texas Children’s Pavilion for Women and Baylor College of Medicine. “And then we have continued evidence that having COVID when you’re pregnant and unvaccinated definitely has worse outcomes for both mom and the pregnancy.”

Pregnant patients are more likely to get seriously ill from COVID, and getting COVID while pregnant increases the chances of giving birth prematurely or losing the pregnancy altogether, . And while the vaccine has been proven to be safe, there’s far less data when it comes to the safety and efficacy of COVID treatments for pregnant women.
“If your thought was, hey, I don’t want to get a vaccine because I don’t want to introduce something into my pregnancy, you’ll be introducing a lot of other things when we have to start treating you for a complicated COVID-19 infection,” said Gandhi.
That’s what Diana found out the hard way when she showed up at the hospital with a headache and fever in her second trimester. She wouldn’t leave the hospital again for nearly five months — and, even her doctors agree, it’s a miracle she left at all.
The worst-case scenario
When Diana got pregnant, she and her husband Chris were thrilled to be adding another child to their growing blended family. Chris works as a deputy with the Harris County Sheriff’s Office, and Diana took care of the four kids they shared, including a now 2-year-old born just a month before the pandemic hit.
Diana’s pregnancy was totally normal. In fact, when she was in her second trimester, she felt well enough to travel so she and Chris went to Las Vegas for their anniversary. When they returned, she had a really bad headache, which her doctors initially chalked up to dehydration.
But then she developed a fever and her oxygen levels started dropping. At the hospital in their suburb north of Houston, they diagnosed her with COVID pneumonia and transferred her to Texas Children’s Pavilion for Women. By the time she got there, she couldn’t breathe.
“The last thing I remember was them telling me that they were going to put me on the ventilator,” she said.

Texas Children’s is a level IV maternal care facility and throughout the pandemic, the staff has cared for a lot of pregnant women battling COVID. The best, and most common, scenario is to deliver the baby before the patient needs to be put on a ventilator or extracorporeal membrane oxygenation (ECMO).
“We’ve had a bunch of 30-, 31-weekers where the baby was delivered prematurely to lift that extra strain for mom,” said Cameron Dezfulian, director of the Adult Congenital Heart Disease ICU at Texas Children’s. “In some of those cases, after the delivery is done, they get so much better by not having that space filled with the baby.”
But Diana was only 18 weeks along. A fetus cannot survive outside the womb before a minimum of 24 weeks of pregnancy. They couldn’t deliver — they were going to have to treat them together.
Doctors put her on a ventilator, but two weeks later, she wasn’t improving. That’s when they started talking to Chris about putting her on ECMO, a last-resort life support machine that would serve as Diana’s lungs outside of her body.
“I did research on that, and it was just bad,” Chris said. “It’s a coin toss if you’re going to live once you get on ECMO, and some of the doctors said it’s less than that.”
There have been only a handful of cases of pregnant patients being put on ECMO to treat COVID, particularly this early in the pregnancy, Dezfulian said.
Diana was sedated, so Chris had to navigate this impossible situation by himself, balancing his wife’s prognosis against the viability of their child, while confronting the very real possibility that neither could be saved.
“I may go home without anything,” he said he remembers thinking. “With a dead baby and a dead wife … there were some really dark days.”

He agreed to put Diana on ECMO, which Dezfulian thought was the best chance to save both mother and baby. And it seemed to be working. She started to improve, enough to come out of sedation, and they got her to 25 weeks of pregnancy, past the point at which the fetus could potentially survive outside the womb.
That was what they’d all been working toward, and yet, even that came with significant complications.
“Once that baby was viable, then all of a sudden, we had to plan for at any moment we might have to deliver him,” Dezfulian said.
They set up the room next door as an obstetrics operating room and had doctors and nurses on stand-by, prepared to deliver, while still hoping to get more time.
“The outcomes get better with every week,” said Dezfulian. “As long as we didn’t think the baby was causing harm to her, we wanted to get them both through as long as possible. She had voiced that from the start, that she wanted to give her baby the best chance possible.”
A turn for the worse
Nearly two months after Diana was admitted, Chris and Dezfulian thought she and the baby had turned a corner. But then, she suddenly had three strokes and a heart attack, while Chris and her father watched.
“Being pregnant, having COVID and being on ECMO are the three major risk factors for blood clots,” Dezfulian said. “COVID also puts you at risk for bleeding. She’d had significant internal bleeding for weeks,” which limited their ability to use blood thinners.

Diana ended up in a coma, and the doctors were back to working without a playbook. Dezfulian met with Chris, took his hand, and they prayed.
“It’s the first time I’ve ever had a doctor pray with me and I didn’t know how to think about that,” Chris said. “Because when a doctor is praying with you, you know there’s not much else … we can do.”
Chris said the doctors told him that they’d see how she was doing in the next seven days.
“I was like, ‘Well, what happens in seven days?’” he remembers asking. “And they just said, ‘We’ll cross that bridge when we get there.’ So that’s when I knew she has to get better this week.”
On the fourth day, Chris took her hand and asked her to give him some sign that she was still there and still fighting. He squeezed her hand. She squeezed back.
“That’s when I knew we were going to get out of there,” he said.
Dezfulian still remembers that moment, and Chris’ certainty that the situation was going to turn around.
“I just felt this sense of reassurance,” Dezfulian said. “Seeing him feel that way and knowing that was coming from his prayers. That made me feel a lot more confident that we were doing the right things.”
Diana continued to improve, and finally, at 31 weeks of pregnancy, she delivered a healthy baby boy by cesarean section. They named him Cameron, after Dezfulian.
“My first response was, I don’t deserve this,” he said. “This was such a team effort. No one physician, nurse or anything can take more than 0.1% credit for this.”

Encouraging others to get vaccinated
In all, Diana spent nearly five months in the hospital, including 51 days on ECMO. She was in and out of sedation and doesn’t remember much about this period, including delivering Cameron.
She didn’t even know she’d given birth until three days after it happened, when a nurse from the neonatal intensive care unit brought him up to visit.
“I was still kind of in and out, so it was kind of blurry for me. … It was really hard to not be in my right mind,” she said. “It was really emotional.”
Cameron was released from the NICU after a month, but Diana stayed in the hospital for several more weeks. She was finally released on Dec. 23, just in time to spend Christmas with her children, who had been looked after by her parents during her five-month hospital stay.
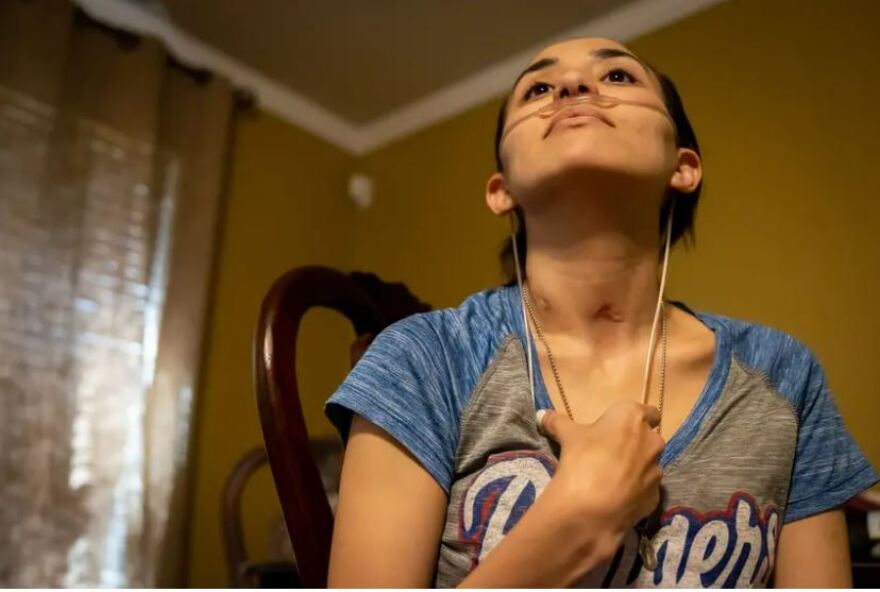
She left the hospital on oxygen, with a chest tube to prevent her lungs from collapsing. She can’t really hold Cameron, because she still doesn’t have full strength in her left arm from the stroke. She’s doing physical therapy five days a week.
And she’s still dealing with the emotional toll of her experience.
“When you’re out of it for so long, you just wake up and [find out] all these things happened to you,” she said. “Every time [Chris] retells the story, there’s something new, like something I hadn’t known before.”
Five days after she was released from the hospital, Diana received her COVID vaccine. She wants other pregnant women to learn from her experience.
“After all I went through, the least of your worries should be the vaccine,” she said. “I put my baby through all this as well.”

Chris got vaccinated, too, when Diana was in the hospital. He’s conservative, and he said when he raises it with his unvaccinated friends and family, he sometimes gets pushback.
“But I’m not getting into politics with them,” he said. “I just say, if you can eliminate what happened to me, if you can do damage control, why not do it? Why risk it like we did?”


